Bone
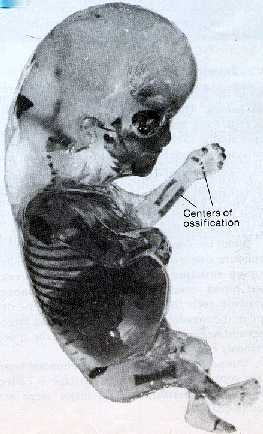
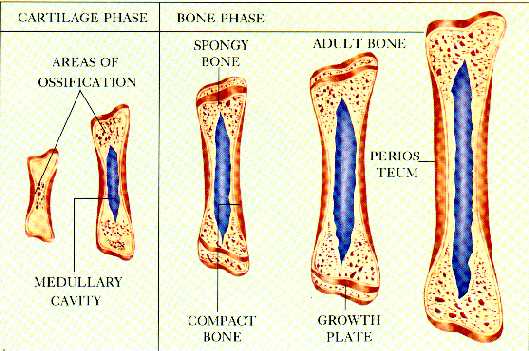
formation (osteogenesis) begins during prenatal development
and persists throughout adulthood. The bones of infants and
children are softer than in adults because it has not yet
been ossified (the process of synthesizing cartilage into
bone). There are two ways in which osteogenesis occurs:
intramembranous ossification and endochondral ossification.
Both types form by replacing existing cartilage however
differ in the method they go about doing it. Two types of
cells that are of great importance in the process are
osteoblasts and osteoclasts. Osteoblasts, used mainly in
intramembranous ossification, are the specialized cells in
bone tissue that deposit calcium into the protein matrix of
bone (collagen). Osteoclasts, used in endochondral
ossification, dissolve calcium previously stored away in bone
and carry it to tissues whenever needed. One third of all of
the bone's components is collagen; a flexible, gelatin-like
matrix. Bones formed during intramembranous formation are
called membranous bones, or occasionally dermal bone, and
bones formed during endochondral formation are called
cartilage bone.
As
seen under a microscope, membranous bones first appear as
flat, membrane-like layers of early connective tissue. These
layers are provided with a constant flow of nutrient blood
supply by networks of blood vessels formed in between the
layers. Early connective tissue cells first arrange
themselves among the layers and then differentiate into
bone-forming cells called osteoblasts. The osteoblasts then
remove calcium from the blood and deposit it among the bone
matrix (the cartilage). As a result, layers of spongy bone
are formed around the original cartilage. Later in
development, spaces among the spongy bone are filled with
bone matrix and become compact bone.
 Osteoblasts continue to
deposit calcium supplements into the matrix until it is
totally surrounded by it. Once this occurs the osteoblasts
are considered to be encased in a lacunae and now called
osteocytes. The original connective cells first formed around
the network of blood vessels are now called the periosteum.
Osteoblasts still not isolated in a lacunae can emerge from
beneath the layer of compact bone and form layers of spongy
bone over compact bone. Examples of intramembranous
ossification are certain broad, flat skull bones.
Osteoblasts continue to
deposit calcium supplements into the matrix until it is
totally surrounded by it. Once this occurs the osteoblasts
are considered to be encased in a lacunae and now called
osteocytes. The original connective cells first formed around
the network of blood vessels are now called the periosteum.
Osteoblasts still not isolated in a lacunae can emerge from
beneath the layer of compact bone and form layers of spongy
bone over compact bone. Examples of intramembranous
ossification are certain broad, flat skull bones.
Endochondral
Ossification-
Endochondral
ossification forms bone by replacing a cartilaginous model,
or precursor, that appeared there earlier in embryonic
development. The cartilaginous models first undergo quick
changes as the connective tissue cells enlarge which in turn
destroys the surrounding 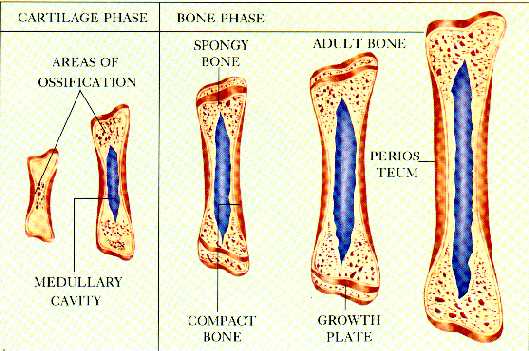 matrix.
Soon after, the connective tissue cells die. While the cells
disintegrate, a periosteum is formed on the outside of the
developing structure (a membrane with many blood vessels).
Next blood vessels and undifferentiated cells raid on into
the disintegrating tissue. Certain connective tissue cells
differentiate and form spongy bone around the previous
template of cartilage.
matrix.
Soon after, the connective tissue cells die. While the cells
disintegrate, a periosteum is formed on the outside of the
developing structure (a membrane with many blood vessels).
Next blood vessels and undifferentiated cells raid on into
the disintegrating tissue. Certain connective tissue cells
differentiate and form spongy bone around the previous
template of cartilage.
Further
growth in cartilage bones occurs once a significant amount of
spongy bone has formed. Thickness in cartilage bones is
accomplished by intramembranous ossification. Just beneath
the layer of periosteum yet above the newly developed spongy
bone, compact bone is formed and hardened with the help of
osteoblasts filling portions of the porous spongy bone with
calcium phosphate crystals (apatite). Sometimes compact bone
is formed on the surfaces of existing bone tissue and they
must be eroded away by specialized cells called osteoblasts.
The crystals of apatite extracted from the bone tissue are
delivered to blood and tissues on demand.
Growth
in the length of bones continues until about the age of 25.
This is possible by an epiphyseal disk. The epiphyseal disk
is found on a portion of the bone that remains cartilaginous.
This portion of the bone, called the epiphysis, are both ends
of the bone that continue to grow throughout development
(lifelong) while the centers of premature bones undergo
ossification. The full length of bone is attained by the
deposition of calcium on the epiphyses.
Healing-
One
of the most widely accepted myths about bone is that it is
dead, unchanging matter. However, your bone is constantly
changing every second of the day as new bone cells replace
old cells, just as your dead skin cells are brushed off but
are continually replaced.
The
healing process of broken bones is also very similar to the
healing process of skin. As soon as a bone breaks, a jacket
of cells forms around the fracture (a broken bone) called a
callus, in the same way skin forms a scab jacket of new cells
around broken skin. Unfortunately, the callus only provides
for protection from infections and such but further damage
can be done if not kept in a cast. A cast is put on to keep
the bone straight while healing and also it is said that by
applying pressure on it the bone heals quicker. Many times
the cast will be put on in such a way that you are still able
to use it. This is because bone, like muscle, grows in
thickness and endurance when used.
Although
bone cells reproduce faster when repairing yet it still takes
a long time to fully heal. In young children, while bones are
still developing, repairs and healing are done fairly
quickly. However as you age, healing tends to take longer. By
adolescence, bones are hardened to an extent so bones are
more complete. Mending in teenagers requires 6-8 weeks in a
cast while after you're 60 or over breaks occur much more
easily. Sometimes just the slightest stress on a bone can
break it, and then repairs are made slowly and sometimes
imperfectly. However, when fractures in bone are healed with
the right amount of time and nutrients to aid in it, the
break or breaks in the bone cannot even be seen with an
x-ray.

Osteoblasts continue to
deposit calcium supplements into the matrix until it is
totally surrounded by it. Once this occurs the osteoblasts
are considered to be encased in a lacunae and now called
osteocytes. The original connective cells first formed around
the network of blood vessels are now called the periosteum.
Osteoblasts still not isolated in a lacunae can emerge from
beneath the layer of compact bone and form layers of spongy
bone over compact bone. Examples of intramembranous
ossification are certain broad, flat skull bones.
 matrix.
Soon after, the connective tissue cells die. While the cells
disintegrate, a periosteum is formed on the outside of the
developing structure (a membrane with many blood vessels).
Next blood vessels and undifferentiated cells raid on into
the disintegrating tissue. Certain connective tissue cells
differentiate and form spongy bone around the previous
template of cartilage.
matrix.
Soon after, the connective tissue cells die. While the cells
disintegrate, a periosteum is formed on the outside of the
developing structure (a membrane with many blood vessels).
Next blood vessels and undifferentiated cells raid on into
the disintegrating tissue. Certain connective tissue cells
differentiate and form spongy bone around the previous
template of cartilage. 
